-
Key things to
do during first 5 minutes of neonatal resuscitation -
Updated NRP
guidelines 2015
http://circ.ahajournals.org/content/132/18_suppl_2/S543.long
-
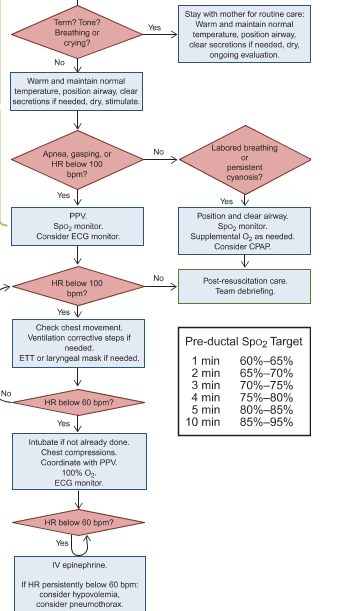
For babies
born precipitously in ED, always ask: 1) Term? 2) Good tone? 3)
Breathing or crying?-
If yes to
all 3Qs, consider delaying cord clamping and hand baby to mother
for skin-to-skin contact while keeping baby warm and dry.-
Clamping of
cord should be delayed 30-60 sec unless child requires immediate
resuscitation -
Associated
with less IVH, NEC, better BPs and blood volume, but a/w more
phototherapy requirement
-
-
If no to any
of Qs, cut cord and begin resuscitation by:-
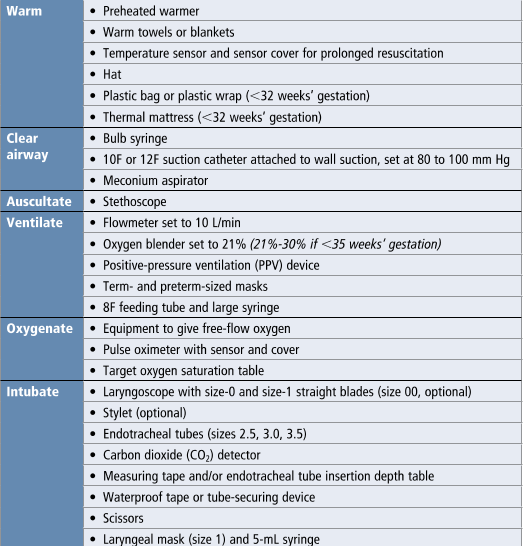
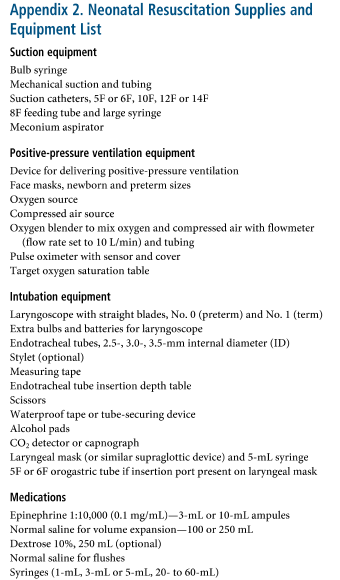
Taking baby
to warmer (make sure it’s on!, plastic bag from neck
down) goal temp 36.5-37.5 -
Bulb
syringe suction to clear secretions, -
Dry,
stimulate. Ventilate/oxygenate as needed. -
Note time,
document APGAR.
-
-
-
Cutaneous
temp monitor on liver – largest organ provides most consistent
measurement. Hypothermia increases risk of intraventricular
hemorrhage, respiratory issues, hypoglycemia, and late onset sepsis. -
Meconium
aspiration no longer empirically intubated, treat similar to other
babies with stimulation, suctioning, PPV as needed. Immediate
intubation thought to delay resuscitation
Resuscitating a neonate: HR, RR, Pox
-
HR:
Detecting HR difficult, 3 lead ECG best, umbilical cord stethoscope
alternate but not as accurate-
If
bradycardic HR <60, start chest compressions, thumb encircling
chest wall, 3:1.
-
-
-
If not
already done, intubate baby -
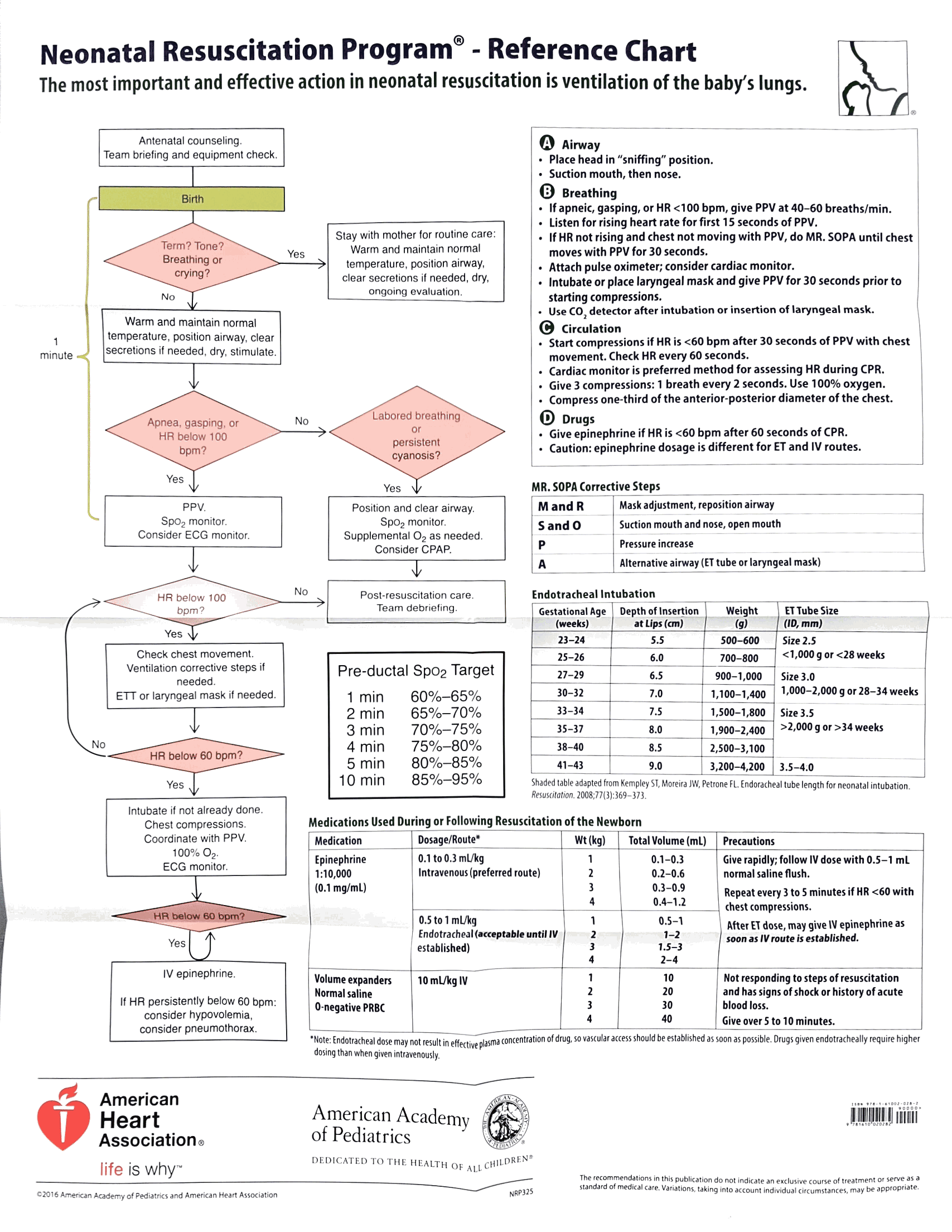
Epi 1:10,000
concentration, dose 0.01 mg to 0.03 mg/kg IV, or 0.05 to 0.1 mg/kg
via ETT
-
-
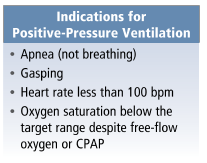
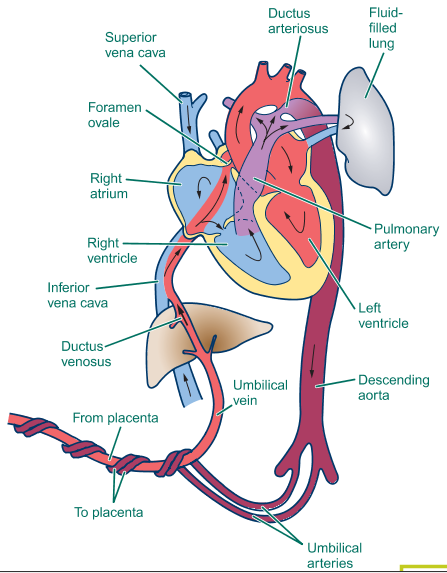
RR/Pulse
ox – low oxygen sat is normal in first few minutes of life.
Increases by 5% every minute of life. Place monitor on R palm/wrist
for pre-ductal measurement, reflects blood that is going to the
brain.-
Normal
preductal (right hand) O2 Sat -
Resuscitation
with room air (FiO2 21%) initially -
Give
supplemental O2 – increase FiO2 if not achieving normal saturation
or has a HR<100. -
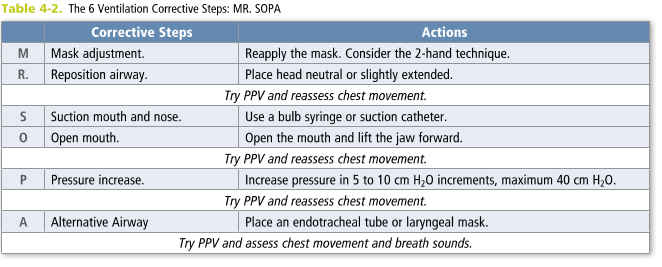
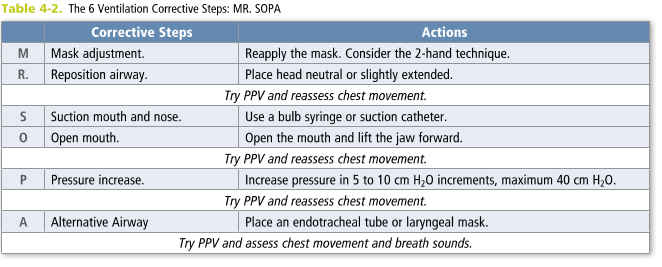
PPV using
BVM to RR 40-60 for 30 sec, CPAP -
If need for
CPR, then intubated baby
-
-
Intubation:
-
ETT = [age/4+4]
Laryngoscope blade
<28 wks 2.5
Pre-term 0
28-34 wks 3.0
Term 1
34-38 wks 3.5
>38 wks 3.5 to 4
PEEP 5
Depth 3xETT size to lip
-
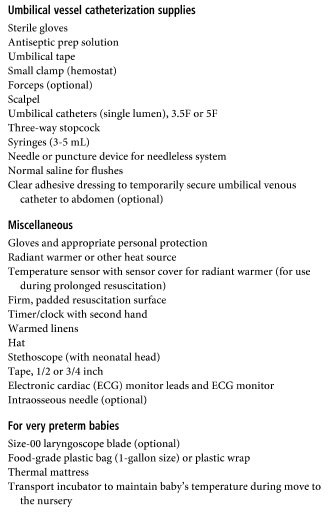
Umbilical
vein catheter: (PED Rm 4 has BOA cart w/ UVC kit)-
http://www.fprmed.com/Pages/Procedures/UmbilicalVein_Cath.html
-
Smiley face:
2 eyes = umbilical arteries, flat mouth = vein. Insert catheter
into vein 2-4cm until blood flow achieved -
DIY UVC kit
– 5 Fr feeding tube, 11 blade scalpel, hemostats, forceps, 3 way
stop cock, 10ml flush, umbilical tie
-
Why does baby
need resuscitation?-
Shock? Blood
or volume? Give transfusion or IVF bolus as indicated, 10ml/kg,
repeat prn -
Uterine
rupture or abruption? -
Accident
with umbilical cord? -
Hypoglycemic?
2ml/kg of D10 as initial bolus, then D10W maintenance IVF at
80ml/kg per day.
-
